EPILEPSY GLOSSARY AND INFORMATION ASSOCIATED WITH THIS NOVEL
*Terms that are italicized are defined elsewhere in this alphabetized glossary.
Age at Onset: childhood had been the most prevalent, but in recent decades we commonly encounter epilepsy developing in the elderly.
This is due to our extended longevity with its attendant increase in strokes, head trauma, brain tumors, and other abnormalities that irritate brain cells and cause brain scars.
Aura: the warning the person perceives that a seizure is starting.
Often it is a mood change, a thought, a memory aberration, or perceiving smells/tastes, sensations or movements. Auras generally last just one or several seconds, but can last many seconds to minutes prior to progressing to the full seizure.
Bathing/Swimming/Athletic Dangers: people suffering from epilepsy should avoid swimming unless someone capable of rescue is present should a seizure occur.
Avoid bathtubs and showers (falling face-
Blank Outs/Staring/Confusion Spells: commonly represents a form of seizure, usually petit mal or complex partial type.
Seizures can be differentiated from normal staring/daydreaming by the difficulty of gaining the person’s attention during a seizure. In addition, the person with mental “blank outs” due to seizures does not have conscious thoughts, but the daydreamer will. During a seizure, the person will neither recall what was said nor be aware of the environment. In order to ascertain whether people actually lost contact with their environment, they may need to be challenged, and tested, by observers (e.g., give the person commands and assess if they’re carried out) since they often deny and are unaware of any loss of contact.
Chewing/Lip-
People in the seizure are unaware of performing these automatisms. Some people move around a room, perform simple actions, cross a busy street or endanger themselves in other ways.
Clues to Suspect Epilepsy: persons presenting with their “first” witnessed seizure may actually have epilepsy, i.e. previous seizures, but be unaware of them.
This is more likely to occur in persons who live or sleep alone. Their only clue may be occasional bed-
Complex Partial Seizure (limbic seizure): altered consciousness (not totally alert) with loss of awareness of surroundings. The person may still respond, but slowly and incompletely (as only looking at people speaking to them, but offering no, or short, and inappropriate responses) with confusion. No recollection of events afterward.
They usually last a few minutes and are preceded by symptoms such as foul smells and/or tastes, and unusual thoughts/memories. These are the aura, the warning of an oncoming seizure. The person may vocalize phrases for which they have no memory, such as “Oh, God! Oh, God!” or “Help me! Help me!” These seizures typically originate within the temporal lobe, which is located at the lower sides of the brain; some begin in a frontal lobe. If the abnormal brain-
Convulsion: this term commonly applies to a grand mal seizure.
These are the second-
CT/MRI Brain Scans: very useful in evaluating causes of seizures. CT (Computerized Tomography) scans require radiation exposure like X-
Each type of scan provides different information about the brain/skull/blood-
Diagnosis: primarily made from the medical history. It is common for the neurological examination and the EEG of persons with epilepsy to be normal. This is because the abnormal brain patterns (epileptiform discharges) and other EEG abnormalities are not always present during the interictal (between seizures) period when most EEGs are done.
Grand mal seizures (convulsive jerking) are readily diagnosed from the person’s history. Petit mal seizures and complex partial seizures require astute history-
Driving Vehicles: not advised. Risks include endangering themselves, passengers and the public if the seizures are not controlled.
Only six of the fifty states (California, Delaware, Nevada, New Jersey, Oregon, and Pennsylvania) mandate all physicians, no matter the specialty, report persons with epilepsy to the Health Department. Other states recommend that these persons assume the responsibility to report the diagnosis, themselves. The Health Departments then notify the Department of Motor Vehicles (DMV) that the person has a condition which could interfere with safe operation of a motor vehicle. The DMV sends medical forms for physicians to complete regarding the condition. The DMV, not the physician, makes the decision to allow, or cancel, the driving privilege. If canceled, the DMV decides how long the person must be seizure-
Electroencephalogram (EEG): painless recording of brain activity. Wires are pasted on the head and connected to the recording machine while the patient rests on a bed. Abnormal brain electrical patterns, i.e. the epileptiform abnormalities (the abnormal brain cell discharges that cause seizures) that are detected in the EEG between seizures (the interictal period) are helpful in diagnosing epilepsy.
A normal test indicates that no abnormal electrical patterns or other changes were detected from the neuron cells’ electrical profile in the cortex during that test period (usually lasting forty-
Epilepsy: a chronic neurological disorder characterized by recurring seizures that are not provoked by any temporary problem in the brain (see “reactive seizures” in Febrile Seizures below). More than one seizure qualifies as epilepsy, even if the incidents are separated in time by years. Epilepsy is a clinical diagnosis; an abnormal EEG is not required for the diagnosis.
The specific abnormality that causes the seizures often cannot be identified; this type of epilepsy is known as primary or idiopathic. Acquired, or symptomatic epilepsy, however, results from identifiable brain abnormalities (often on brain scans), such as brain injuries and brain malformations, strokes, tumors, infections, drugs and toxins, alcohol, hormonal changes (including menstruation, called catamenial epilepsy) and metabolism disorders. In general, inherited epilepsy is not common. Approximately one percent of the population of the United States has epilepsy.
Febrile Convulsions: most commonly occurs in children aged several months up to five years old. Typically these occur in the beginning of a fever (febrile illness) and they are usually not associated with any serious cause.
They don’t require anticonvulsant medications, and they don’t recur during that febrile illness. They are reactive seizures, i.e., they react to the fever-
Hallucinating Smells/Tastes: common as part of the initial aura, especially in complex partial epilepsy. Patients will perceive odors—usually foul (classically “burning rubber”)—that no one else in their environment can smell.
If physicians fail to ask about these symptoms, patients suffering their “first” observed seizure, or confusion episode, commonly do not mention them. Non-
Juvenile Myoclonic Epilepsy: sudden, quick jerks on both sides of the body beginning in late-
These seizures can be a single jerk, or repetitive jerks, usually without loss of awareness, that occur shortly after morning arousal. A common symptom is an exaggerated startle reaction, such as the child involuntarily “throwing” something, like the breakfast-
Petit Mal Epilepsy (absence): petit mal seizures consist of staring spells with loss of awareness, eye-
Patients are typically unaware of having lost contact with their surroundings. They will commonly ask companions to repeat what was just said. When the seizures are unrecognized, observers may consider these people as “ditzy,” or odd, due to their periodic mental dullness. The specific petit mal EEG abnormality is a three-
Postictal Confusion: the groggy/confusion period immediately following convulsions and complex partial seizures.
It routinely lasts minutes to hours, and people commonly fall asleep. Strangers, unfamiliar with the person’s diagnosis typically call for emergency personnel/ambulances when they observe the convulsion and/or postictal confusion and sleepiness. Once hospital personnel learn that a previous epilepsy diagnosis has been made, they will discharge the patients home once they are alert.
Psychogenic Seizures/Pseudoseizures: these can resemble true seizures to the observer, but they are not. These events have a psychological cause that is often associated with some underlying, subconscious, secondary gain or conscious malingering.
Anticonvulsant medications (see Treatment) fail to prevent them, but psychiatric treatment that targets the psychogenic cause of the seizure can be beneficial. The EEGs performed during overt “seizures” remain normal, so videotaping the patient’s behavior is helpful for making this diagnosis. Pseudo-
Psychosocial Adjustment to Epilepsy: leading full and independent lives can be a challenge in epilepsy, especially for those people who have incomplete seizure control.
School/employment opportunities, marriage, family and social life, driving, and athletic participation all must be addressed. Epilepsy Foundations/Societies help people find local epilepsy-
Seizure (ictus): a sudden, temporary, uncontrolled disruption of electrical activity of brain cells (neurons) that interfere with normal brain function. Seizures are not a disease, but are the representative expression of the disease causing the seizure.
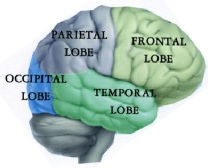
The site of this abnormal activity determines the form of the seizure.
Frontal lobe (the anatomical front of the brain) seizures can cause jerking movements and postural changes (e.g., falling down), or emotional changes and speech problems.
Occipital lobe (the anatomical back of the brain) seizures can cause visual symptoms such as blind spots and flashes.
Parietal lobe (the sides of the brain) seizures can cause numbness, tingling, pins-
Temporal lobe (lower side of brain) seizures can cause emotional or psychological phenomena, fear, and hallucinations.
A single seizure occurs in an estimated eight to ten percent of the population for undetermined reasons and then never recurs during their lifetimes. Fevers in young children; sleep deprivation (usually more than thirty-
Simple Partial Seizure: clear consciousness is preserved during the seizure.
These patients can communicate and remain aware of their surroundings with full recollection of events despite seizure-
Spinal Tap (lumbar puncture): This procedure is useful to diagnose central nervous system (CNS) infections, inflammation, cancers, bleeding, abnormal pressure within the central nervous system, multiple sclerosis, peripheral nerve disease, and other conditions. The spinal tap is usually far less unpleasant than patients expect it to be when it is performed by an experienced physician. Ideally, the test is completed in less than thirty minutes and can be done as an out-
Typically, the local anesthetic is the most uncomfortable part of the procedure. It is injected within the skin layers, which stretch apart; this causes a burning sensation. Next, the spinal needle is directed deeper into the space between the spinal vertebrae and into the spinal canal; this is usually painless. Pressure within the central nervous system is measured, and then cerebrospinal fluid is collected as it drips from the end of the hollow needle into test tubes. The red-
Status Epilepticus: occurs when the seizure activity recurs, and lasts longer than ten minutes without the person regaining full consciousness between seizures.
This is a serious medical emergency that requires immediate medication, breathing and medical-
Sudden Unexpected Death during Seizures: very rare.
Theories about this phenomenon consider changes in the brain’s regulating centers for breathing and heartbeat. In this case the person is often found dead in bed with no identifiable cause.
Tongue Swallowing During Seizure: this does not happen.
Treatment: the goal is complete cessation of seizures.
If the most appropriate anticonvulsant (medications to stop seizures) medication is administered at the “correct” dosage, approximately fifty percent of people with epilepsy will gain complete control of their condition without having any more seizures as long as the medication is taken as prescribed. Determining the “most appropriate” medication in the “correct” dosage is a trial-
Following is a list of commonly prescribed anticonvulsant medications, by brand and generic names: Depakote (Divalproex), Dilantin (Phenytoin), Keppra (Levetiracetam), Klonopin (Clonazepam), Lamictal (Lamotrigine), Lyrica (Pregabalin), Mysoline (Primidone), Neurontin (Gabapentin), Phenobarbital, Tegretol (Carbamazepine), Topamax (Topiramate), Trileptal (Oxcarbazepine), Zarontin (Ethosuximide), and Zonegran (Zonisamide). Generally, if seizures persist while the patient is taking a specific medication, the dosage is increased until seizures are controlled or side effects can’t be tolerated. Other anticonvulsants are then added, or substituted. This is the “art” in the practice of medicine. This process can take many months of trial and error.
Another twenty to thirty percent of people with epilepsy will gain incomplete seizure control; they may experience an infrequent seizure despite trying many of the current anticonvulsants. A further twenty percent have uncontrolled seizures despite all anticonvulsant trials. Surgical removal of the seizure-
Treatment Cessation: epilepsy that begins in the late teens, and later, generally requires lifelong treatment with anticonvulsant (see Treatment) medications. The medical profession cannot cure epilepsy.
Epilepsy is considered to be “inactive” or “cured” under certain circumstances: no seizures for two years; the physical examination, EEG, brain scan, and pertinent laboratory blood tests are all normal. It would be prudent to ascertain that the EEG is still normal before tapering the patient off of the anticonvulsant. Before commencing the discontinuation process, patients should strongly desire to stop their medications, and they must be aware that driving privileges would again be withdrawn if another seizure occurs. Adults, whose epilepsy began after their teenage years, will frequently experience a return of seizures within weeks to years after stopping their medications; this is unpredictable. If this scenario occurs, they may then be convinced that medications will be required, most likely, for life.
Violent Behavior during Seizures: this is most associated with complex partial seizures. People who are physically restrained while suffering a complex partial seizure often involuntarily strike out.
Planned violent or criminal behavior during a seizure does not occur in the real world, despite what popular novels and movies would have us believe. The violent response to the restraint is a non-